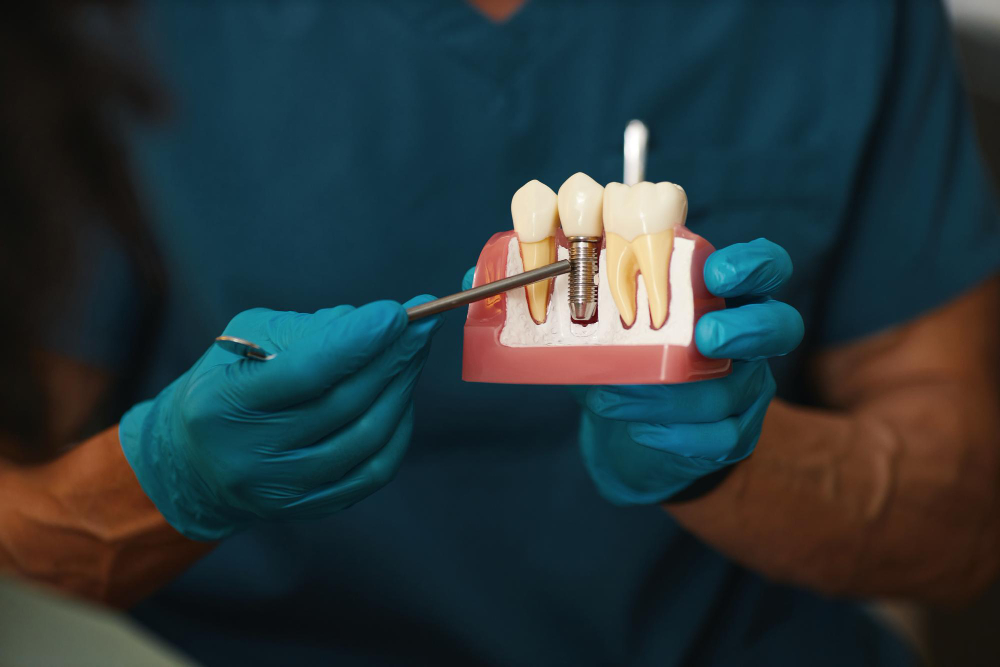
Dental implants have become the gold standard in restoring missing teeth, offering patients a permanent, functional, and aesthetically pleasing solution. However, for a dental implant to be successful, it requires a solid foundation — the jawbone. Without adequate bone volume and density, implant placement may not be possible. This is where bone grafting in dental implantology plays a crucial role.
Bone grafting is a procedure used to augment or rebuild areas of the jaw that have been compromised due to tooth loss, injury, or other factors that cause bone resorption. In dental implantology, bone grafting is often a prerequisite for a successful implant placement, as it ensures that there is sufficient bone for the implant to integrate properly.
In this article, we’ll explore the importance of bone grafting in dental implants, how the procedure works, the different types of bone grafts, and how advancements in bone grafting techniques are improving implant outcomes.
Why Bone Grafting is Necessary in Implantology
The success of dental implants is largely dependent on the process of osseointegration, which is the fusion of the implant with the surrounding jawbone. This process requires a stable and healthy bone structure to anchor the implant securely. When the jawbone has deteriorated due to tooth loss, trauma, or periodontal disease, there may not be enough bone to support the implant. Without sufficient bone mass, the implant is at risk of failure.
Bone loss typically occurs after the loss of a tooth. The natural process of bone resorption begins as soon as a tooth is lost, as the bone no longer receives stimulation from the tooth root. This leads to a gradual reduction in bone volume and density. Over time, the jawbone may shrink, creating areas of weakness or voids that make it challenging to place implants. This is where bone grafting comes in.
Bone grafting allows the dentist or oral surgeon to restore or augment the jawbone so that it can support dental implants. By rebuilding the bone structure, bone grafting increases the chances of successful implant placement, enabling the patient to benefit from the long-term advantages of dental implants.
How Bone Grafting Works
The bone grafting process involves the surgical placement of bone material into areas where bone loss has occurred. This material acts as a scaffold that promotes the growth of new bone tissue. Over time, the body will integrate the grafted material with the natural bone, filling the void and creating a solid foundation for the dental implant.
The procedure can be done in conjunction with the implant placement or as a separate procedure prior to implant placement. In some cases, bone grafting may be necessary to rebuild the bone before an implant can be placed, while in other cases, it may be performed at the same time as implant surgery. The choice of whether to perform bone grafting as a standalone procedure or as part of the implant placement depends on the extent of bone loss and the specific needs of the patient.
Types of Bone Grafts
There are several types of bone grafts, each with its own indications, benefits, and limitations. The type of graft chosen depends on the patient’s needs, the area of the jaw being treated, and the extent of the bone loss. The main types of bone grafts are:
1. Autografts
Autografts are bone grafts taken from the patient’s own body. These grafts are typically harvested from areas such as the chin, jaw, or hip. Autografts have the advantage of being biocompatible because they come from the same patient. This reduces the risk of rejection and promotes faster integration with the existing bone. Since autografts are rich in growth factors, they tend to offer a high success rate.
However, autografts require an additional surgical site to harvest the bone, which can increase the complexity of the procedure and the recovery time. Patients may also experience some discomfort at the donor site. Despite these drawbacks, autografts are considered the “gold standard” in bone grafting because of their excellent healing potential.
2. Allografts
Allografts are bone grafts taken from a donor, typically a cadaver or a living donor. These grafts are processed and sterilized before being used in the recipient. Since allografts come from a different individual, there is a small risk of immune rejection or disease transmission, although this risk is minimized through extensive screening and processing.
Allografts are a popular choice because they eliminate the need for a second surgical site, reducing the overall procedure time and discomfort for the patient. While they may not offer the same regenerative potential as autografts, they still provide a strong scaffold for new bone growth and are commonly used in dental implantology.
3. Xenografts
Xenografts are bone grafts sourced from animals, usually cows or pigs. These grafts undergo a special processing technique to make them biocompatible for human use. Like allografts, xenografts eliminate the need for a second surgical site and can be a suitable alternative when autografts are not feasible.
Xenografts are often used as a temporary solution that is eventually resorbed by the body and replaced by new bone. While they provide a solid framework for bone regeneration, they do not offer the same growth factor stimulation as autografts, and patients may require additional grafting procedures in the future.
4. Alloplasts
Alloplasts are synthetic bone grafts made from biocompatible materials such as hydroxyapatite or calcium phosphate. These materials mimic the natural composition of bone and encourage the growth of new bone tissue. Alloplasts are typically used in cases of mild to moderate bone loss, and they can be a good option when biological grafting materials are not available or suitable.
Since alloplasts are synthetic, they do not carry the same risk of disease transmission or rejection as allografts or xenografts. However, they may not be as effective at stimulating bone growth, and they may not integrate as well with the natural bone as autografts.
5. Bone Substitutes
In some cases, a combination of materials, including bone substitute materials, can be used to enhance the success of bone grafting procedures. Bone substitutes are often used to support bone regeneration when there is a need for added volume or strength. These substitutes may be made of synthetic or natural materials and are commonly used in conjunction with other types of bone grafts.
The Bone Grafting Procedure
The bone grafting procedure is typically performed under local anesthesia, though sedation or general anesthesia may be used depending on the complexity of the case and the patient’s preferences. Here is a general overview of the bone grafting process:
- Consultation and Evaluation: The first step is a thorough consultation with the dentist or oral surgeon, who will evaluate the patient’s oral health and assess the extent of bone loss. Digital imaging, such as X-rays or CT scans, is often used to determine the best approach for grafting.
- Preparation: Once the type of bone graft is determined, the patient will be prepared for surgery. The surgeon will numb the area where the graft will be placed, and if an autograft is being used, the bone will be harvested from the donor site.
- Grafting: The graft material is carefully placed into the bone-deficient area of the jaw. The surgeon may use screws, plates, or membranes to secure the graft and prevent movement. The graft is then covered with a protective layer, and the surgical site is sutured closed.
- Healing: After the procedure, the grafted bone will undergo a healing process that typically takes several months. During this time, the body integrates the graft material with the surrounding bone, promoting new bone growth.
- Implant Placement: Once the graft has fully integrated, dental implants can be placed. The newly regenerated bone provides a solid foundation for the implants, allowing for successful osseointegration and long-term implant stability.
Advancements in Bone Grafting Techniques
Over the years, there have been significant advancements in bone grafting techniques, which have improved the success rates of dental implant procedures. Some notable developments include:
1. Minimally Invasive Surgery
Minimally invasive techniques have been developed to reduce the size of the incision and the amount of tissue manipulation required during bone grafting. These techniques result in less postoperative discomfort, reduced swelling, and faster recovery times.
2. Growth Factors and Platelet-Rich Plasma (PRP)
The use of growth factors and PRP (platelet-rich plasma) has enhanced the bone regeneration process. By concentrating platelets from the patient’s own blood, PRP accelerates healing and promotes bone growth. This can improve the success of bone grafting and shorten recovery times.
3. 3D Imaging and Guided Surgery
Advances in 3D imaging and guided surgery have made bone grafting more precise. With 3D imaging, dentists and oral surgeons can plan the grafting procedure with high accuracy, ensuring that the graft material is placed in the most optimal location for implant placement.
Conclusion
Bone grafting is an essential component of modern dental implantology, providing the foundation needed for successful implant placement. Whether a patient has experienced bone loss due to tooth extraction, periodontal disease, or trauma, bone grafting can restore lost bone and ensure the long-term success of dental implants. With advancements in materials, techniques, and technology, bone grafting continues to improve, offering patients a reliable solution for restoring their smiles and their oral health.
If you are considering dental implants but have concerns about bone loss, bone grafting could be the solution you need. By consulting with an experienced implantologist or oral surgeon, you can determine the best approach to rebuilding your jawbone and achieving a successful and lasting implant restoration.




